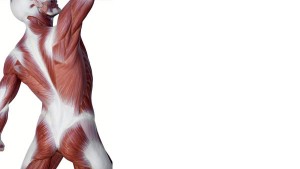
 Ok, get ready. There is some mind numbing anatomy later in this post. But I want to tell you that it is all going to end up at a place where we can make sense of it. Of course for that to happen you might have to pull out 2 or 3 anatomy books. But this intense focus on this anatomy relates to what we can do in the studio.
Ok, get ready. There is some mind numbing anatomy later in this post. But I want to tell you that it is all going to end up at a place where we can make sense of it. Of course for that to happen you might have to pull out 2 or 3 anatomy books. But this intense focus on this anatomy relates to what we can do in the studio.
In a previous post I promised to talk about the Thoracolumbar Composite (TLC) and its importance to our work as movement therapists and to our understanding of our amazing fascial body suit.
I want to start with four basic , foundational concepts or principles that my mentor, Marie Jose Blum , has been telling her students for the past 20 yrs…
a) With a neutral position of the pelvis , the bones narrow but the tissue widens. Just stay with me…
b) Our inner corset mechanics work because the fascia is a shared entity especially the line of the deep Transverse abdominals and the deep spinal muscles. So the front hip bones can come closer together and the sit bones can widen without destabilizing the sacrum because of this continuity of tissue.
c) The Transverse Abdominis (TrA) is a important structure and worth getting familiar with. It is a important feed forward mechanism in conjunction with its core conspirators.
In my next post I will talk more about the Transverse and its many attributes. Not enough time here.
d) The multifidus is the lifeline of what is holding us from deep inside.
I wanted to begin with that because the difficult anatomy that we are about to dive into scientifically proves what MJ has been teaching us through movement all these years.
In Dr. Andry Vleeming’s lecture, study and article “The thoracolumbar fascia : anatomy, function and clinical considerations ” in the Journal of Anatomy (2012), he goes into depth about the TLC and its importance in our ease of movement and stability along with the rest of the TLF and its tissue partners in crime.
Forgive me for what you are about to deal with here – but I beg you to keep going…
The posterior layer of the TLF ( thoracolumbar fascia) is divided into a superficial and deep laminae. The deep portion of this posterior layer is a retinacular sheath surrounding the paraspinal muscles (The iliocostalis, longissimus and multifidus) This deep laminae of the posterior layer of the TLF has been labeled the Paraspinal Retinacular Sheath (PRS). To the lateral potion of this sheath (around the paraspinal muscles), there is a thickening of the connective tissue and this is the point where the PRS joins with the aponeurosis of the deep abdominals, the Transverse Abdominals. Yes! This connection has been known for a long time but Vleeming’s new insight and detail on this subject and the fine mechanics of this area are incredible. If you want more read the article.
Ok, come up for air and dive back in to the depths…
Below the level of L4-L5 where the aponeurosis of the erector spine and multifidus muscles become thicker , Dr Vleeming states : “The aponeurosis of the erector spinae fuses to the posterior overlying deep lamina and the superficial lamina (this is the posterior layer of the TLF) to form an inseparable composite, termed the TLC. The TLC adheres tightly to the PSIS (posterior superior iliac spine) and the border of the sacrum. It then covers the sacrotuberous ligaments eventually reaching the ischial tuberosities.” Yes! So it makes even greater sense that when we activate our Inner Corset and the top of the pelvis narrows and the bottom widens that the sacrum can stay secure and the SI joints are not unstable. Of course this is the optimal and original design of our bodies and the way it should function. We all know clients and teachers alike that have very unstable and/or unyielding Sacroiliac (SI) joints. Keep reading, you will find some clues on how to balance that for yourself and your clients!
It is well known and studied that the Transverse Abdominis and Oblique muscles create a force closure of the sacrum and ilium thereby stabilizing the pelvis in an upright position by pulling the ASIS’s ( anterior superior iliac spines) of the ilium towards each other. But what is preventing the back of the ilium from moving laterally and destabilizing the sacrum and opening the posterior aspect of the sacroiliac ( SI) joints? I know I already answered that above but I want to kind of hit you over the head with this. Sorry…
The TLC (thoracolumbar composite) is key for the job of resisting the lateral movement of the back of the pelvis when the front hip bones move closer together. The PSIS ( on the back of the ilium) is anchored by the TLC and because of this a contraction of the Transverse Abdominis is able to help compress the SI joints and create a force closure securing the sacrum. It seems that the shared connective tissue plays a huge part in how we function, transfer load and work share in the body. Vleeming states ” It has been demonstrated that active muscles will transfer forces outward as well as longitudinally and therefore deform their associated connective tissues, depending on the magnitude and direction of forces generated (Brown & McGill, 2009). Huijing (2003) and Aspden (1990) have shown that muscle force transmission is not exclusively a serial process from muscles fibers to tendon, but that an additional lateral component of transmission occurs through the surrounding connective tissue connections.” Ahh, the fascia …
Vleeming also points out that this structure working in an optimal way is also governed by the optimal mechanics of the Multifidus which he calls a “hydraulic amplifier mechanism “. He states that a weakening or fatty involution of the multifidus structure creates a unstable environment for the whole area of the lower back and pelvis. The multifidus is the lifeline of our inner structure and is greatly ignored. When we are young our spring system and inner corset works naturally for us up to a point. If we overuse or under-use our system imbalance reigns. We mostly tend to live in our outer corset , in our extrinsics, and structures that live in our deep body and are suppose to hold us from inside go to sleep and sometimes seem to disappear. As we grow older without these deep structures hugging us we break down.
The good news is that we as Movement and Pilates professionals have tons in our tool box to help bring back the biomechanics we were born with. Part of my point in this post is to say ” We as contemporary Pilates instructors have been paying attention to all of what Dr Vleeming is talking about for years and years. And now it is great to get validation for what we have intuitively known and that we are helping our clients come back to what is natural and right for the human body. This type of movement and awareness of anatomy brings us closer to who we truly are and is our birthright.” It is exciting and there is so much information to bathe in. Let me know your thoughts and discoveries.
Whew, you made it to the end!
~Jennifer




Leave A Reply (8 comments So Far)
Please - comments only. All Pilates questions should be asked in the Forum. All support questions should be asked at Support.
You must be logged in to post a comment.
Jen! Fabulous! Can I just say I love working everyday with such a brilliant inspiring teacher!
I feel the same way about you sister!
Fascinating!
There are always so many things to learn about the inner workings of the body… We will never get bored in this line of service!
Brilliant!!This is a clear and (whew)exhaustive explanation. Thank you.
Hi Brenda!
So happy you enjoyed this post.
Love
Jen
Hi Jen,
Can you help me with the whole bracing theory? For a very rigid brace, Stuart McGill states that one should bulge or pop the belly outwards. I have often heard this from other professionally qualified people. I damaged my back while lifting something many years back using this theory. I now look at it from a lift of the pelvic floor and a corseting in with a slight resistance to the corseting in. Is this how you would describe it?
Also, I wonder why so many people with such indepth knowledge and experience describe strong bracing as a bulging or popping outward. Aren’t one directional forces unstable?
Can you describe the muscle mechanics of this action from the deep core then outwards to the more superficial stabilisers which will help me visualise? Maybe the Transverses Abdominus corsets in while the Rectus Abdominus and External Obliques create a sense of outward bulging while in an isometric contraction. What are your thoughts about this?
I would love to hear from you. 🙂
Hi Candace,
It is great hearing from you. I love your thought process and it really seems you have answered your own question. You are on the right track. Our core needs to be responsive and it needs to respond appropriately to the task at hand. So it needs lots of options. I think you would really enjoy any of Marie Jose Blom’s workshops on the site.
Love
Jen